Personality disorders (PDs) are mental disorders with extreme personality traits that interfere with a person’s everyday life. Although personality disorders are long-term mental conditions, their symptoms can be effectively managed with therapy, medication, and self-help strategies.
What Is A Personality Disorder?
Personality disorders occur when certain troubling personality traits make it difficult for a person to function normally. They majorly involve maladaptive and chronic patterns of cognition, behavior, and mood. These conditions often last for a lifetime, creating difficulties in work, social life, and personal life.
The types, causes, and symptoms of personality disorders are overarching and research 1 Newlin, E., & Weinstein, B. (2015). Personality disorders. Continuum (Minneapolis, Minn.), 21(3 Behavioral Neurology and Neuropsychiatry), 806–817. https://doi.org/10.1212/01.CON.0000466668.02477.0c is still trying to understand the different personality disorders and their well-categorized diagnosis and treatment. Personality disorders are common but long-term and complex. They are frequently associated 2 Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235 with an inferior quality of life (QoL), poor health, and premature mortality. These mental conditions can be distressing for the suffering individual, the people around them, as well as society as a whole.
People suffering from personality disorders may experience emotional dysfunction and perceive reality in distorted ways. They may also suffer from low self-esteem and self-confidence, and project their insecurities on others. These factors affect their normal emotional responses and conduct. They tend to experience extreme negative emotions like:
- Suspicion
- Narcissism
- Mistrust
- Impulsivity
- Malice, etc.
This contributes to their extremely poor social lives, characterized by unstable and toxic relationships. If left untreated, personality disorders can severely impact a person’s personal and professional relationships and social functioning.
However, they can be addressed in the long run with timely diagnosis, the right treatment, and a disciplined therapeutic regime. Luckily, certain personality disorders phase out as the individual ages. The symptoms become less severe and debilitating with age.
Read More About Narcissism Here
How Common Are Personality Disorders?
Personality disorders are quite common. According to the WHO 3 Fariba KA, Gupta V, Kass E. Personality Disorder. [Updated 2022 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556058/ , the worldwide prevalence of personality disorders is said to be 6.6%. The prevalence of the three separate clusters (A, B, and C) is 3.6%, 1.5%, and 2.7%, respectively.
Research 4 Sansone, R. A., & Sansone, L. A. (2011). Personality disorders: a nation-based perspective on prevalence. Innovations in clinical neuroscience, 8(4), 13–18. shows that the prevalence of personality disorders varies with age, gender, ethnicity, and cultural background. In fact, studies 5 Tyrer, P., Mulder, R., Crawford, M., Newton-Howes, G., Simonsen, E., Ndetei, D., Koldobsky, N., Fossati, A., Mbatia, J., & Barrett, B. (2010). Personality disorder: a new global perspective. World psychiatry : official journal of the World Psychiatric Association (WPA), 9(1), 56–60. https://doi.org/10.1002/j.2051-5545.2010.tb00270.x show that personality disorders are most common in:
- The young
- The unmarried
- The socially and economically disadvantaged
- People with inadequate education
- The incarcerated population
- People with existing mental illness
Symptoms Of A Personality Disorder
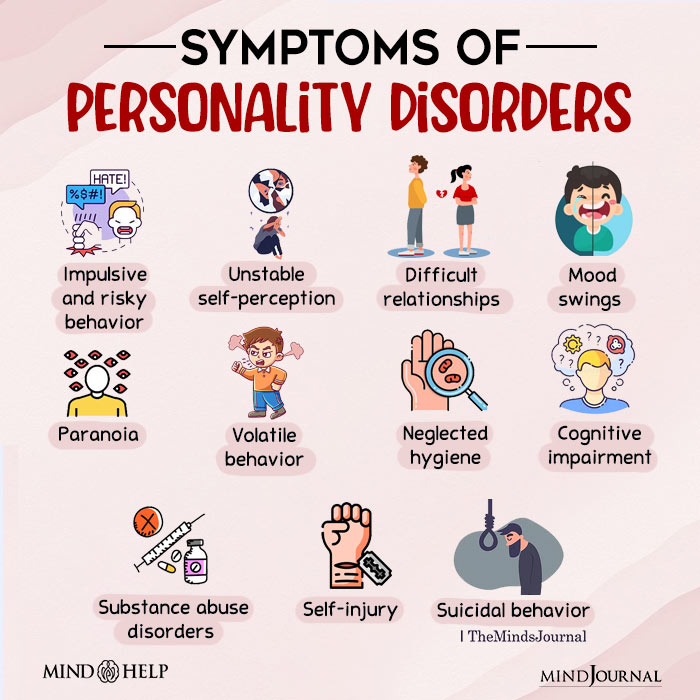
Depending on the type, personality disorders may have different symptoms. 6 Fariba KA, Gupta V, Kass E. Personality Disorder. [Updated 2022 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556058/ Some of them include:
- Impulsive and risky behavior (such as gambling, sex addiction, binge eating, etc.)
- Unstable or fragile self-perception
- Unstable and difficult relationships
- Mood swings
- Paranoia
- Volatile behavior
- Neglected hygiene
- Cognitive impairment (particularly amnesia)
- Substance abuse disorders
- Self-injury
- Suicidal behavior
Read More About Paranoia Here
Types Of Personality Disorders
In the DSM-5, the personality disorder types are divided into 3 clusters—depending on the symptoms and the severity of the personality disorders. Provided below is a list of personality disorders, with the major cluster groups and their sub-categories:
1. Cluster A
Personality disorders in cluster A are disorders defined by odd or eccentric behavior. This group of disorders is greatly associated with schizophrenia and it shares similar schizoaffective symptoms like:
- Distorted reality
- Hallucinations
- Eccentric behavior
- Difficulty in maintaining relationships
- Experiencing paranoia and other irrational fears
- Vulnerability to psychosis and schizoaffective disorders
The three types 7 Esterberg, M. L., Goulding, S. M., & Walker, E. F. (2010). Cluster A Personality Disorders: Schizotypal, Schizoid and Paranoid Personality Disorders in Childhood and Adolescence. Journal of psychopathology and behavioral assessment, 32(4), 515–528. https://doi.org/10.1007/s10862-010-9183-8 of personality disorders in cluster A include:
I. Paranoid personality disorder (PPD)
People suffering from paranoid personality disorders usually experience feelings of extreme mistrust and irrational suspicion. They also experience anger over presumed abuse, anxiety over perceived threats, and a heightened sense of fear.
II. Schizoid personality disorder (PD)
People with schizoid PD display odd behavior related to personal detachment, social avoidance, and apathy. They are restricted in their emotional expressions and they tend to avoid intimacy. Mostly, they are characterized by a lack of interpersonal relationships.
III. Schizotypal personality disorder (SPD)
People with schizotypal PD are characterized by odd beliefs, thinking, and speech. The hallmark of SPD is paranoia and its sufferers tend to experience paranoia-related social anxiety.
2. Cluster B
Cluster B 8 Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235 personality disorders are characterized by dramatic, impulsive, and extremely emotional behavior. People with these personality disorders are characterized by impulsive, self-destructive, and emotional behavior and incomprehensible social interactions.
The most common personality disorders in cluster B include:
I. Antisocial personality disorder
Dissocial or antisocial PD involves a disregard for social rules and social norms and a lack of empathy for others. People with antisocial PD usually harbor a grandiose self-image and display aggressive and manipulative behavior. Research 9 Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235 affirms that they are also the ones with criminal and psychopathic tendencies.
II. Borderline personality disorder (BPD)
Borderline personality disorder (BPD) is a psychiatric disorder in which the person suffers from unstable relationships, a distorted sense of self and reality, and emotional dysfunction.
III. Histrionic personality disorder
Histrionic personality disorder is a psychiatric disorder in which a person displays extremely erratic, emotionally charged, and attention-seeking behavior.
IV. Narcissistic personality disorder (NPD)
People with narcissistic personality disorder (NPD) 10 Kacel, E. L., Ennis, N., & Pereira, D. B. (2017). Narcissistic Personality Disorder in Clinical Health Psychology Practice: Case Studies of Comorbid Psychological Distress and Life-Limiting Illness. Behavioral medicine (Washington, D.C.), 43(3), 156–164. https://doi.org/10.1080/08964289.2017.1301875 are characterized by grandiosity, fantasies of unlimited power or importance, and the need for admiration or special treatment. They also display extremely high levels of paranoia and psychopathy.
Read More About Cluster B Personality Disorders Here
3. Cluster C
The characteristics of personality disorders in cluster C are anxiety or fear-related. These disorders include:
I. Avoidant personality disorder (AVPD)
Avoidant personality disorder (AVPD) is associated with emotional distress, cognitive impairment, and disability. People with this type of disorder tend to isolate themselves and avoid duties and responsibilities. They are also extremely sensitive to criticism and rejection.
II. Dependent personality disorder
Dependent Personality Disorder (DPD) is a long-term condition 11 Ramsay, G., & Jolayemi, A. (2020). Personality Disorders Revisited: A Newly Proposed Mental Illness. Cureus, 12(8), e9634. https://doi.org/10.7759/cureus.9634 that involves pervasive mental and emotional dependence on others. Sufferers rely on other people for comfort, reassurance, advice, and support. They suffer from a chronic fear of abandonment and have trouble making simple everyday decisions.
III. Obsessive-compulsive personality disorder (OCD)
People with OCD or anankastic PD tend to compulsively focus on orderliness and perfectionism. They observe very rigid conformity to rules and are prone to controlling others around them to the point of satisfaction.
What Causes Personality Disorders?
There is no specific reason for the development of personality disorders. However, research 12 Sansone, R. A., & Sansone, L. A. (2011). Personality disorders: a nation-based perspective on prevalence. Innovations in clinical neuroscience, 8(4), 13–18. attributes the common causes of personality disorders to:
- Genetic mechanisms 13 Nigg, J. T., & Goldsmith, H. H. (1994). Genetics of personality disorders: perspectives from personality and psychopathology research. Psychological bulletin, 115(3), 346–380. https://doi.org/10.1037/0033-2909.115.3.346 and birth deformities
- Traumatic brain injury 14 Burns, S., Kappenberg, R., McKenna, A., & Wood, C. (1994). Brain injury: personality, psychopathology and neuropsychology. Brain injury, 8(5), 413–427. https://doi.org/10.3109/02699059409150993
- Personality traits 15 Widiger, T. A., Crego, C., Rojas, S. L., & Oltmanns, J. R. (2018). Basic personality model. Current opinion in psychology, 21, 18–22. https://doi.org/10.1016/j.copsyc.2017.09.007 like narcissism, aggression, suspicion, etc. add to the risk of PDs
- A history of childhood abuse and trauma
- A history of parental abuse, neglect, and abandonment
- A family history of mental disorders
- Negative developmental experiences 16 Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235 (related to war, poverty, etc.)
- Certain cultural and societal norms 17 Alarcón, R. D., & Foulks, E. F. (1995). Personality disorders and culture: contemporary clinical views (Part A). Cultural diversity and mental health, 1(1), 3–17.
- Stress 18 Candrian, M., Schwartz, F., Farabaugh, A., Perlis, R. H., Ehlert, U., & Fava, M. (2008). Personality disorders and perceived stress in major depressive disorder. Psychiatry research, 160(2), 184–191. https://doi.org/10.1016/j.psychres.2007.06.014 (like workplace demands, bullying, workaholism, etc.)
- Major life changes (like the death of a loved one, experiences of relocation, etc.)
How To Diagnose Personality Disorders?
The criteria to diagnose personality disorders have been laid down by psychiatric manuals like ICD and DSM. These disorders can be easily categorized and diagnosed on the basis of their symptoms, severity, and longevity. The process of diagnosing personality disorders 19 Hopwood, C. J., Kotov, R., Krueger, R. F., Watson, D., Widiger, T. A., Althoff, R. R., Ansell, E. B., Bach, B., Michael Bagby, R., Blais, M. A., Bornovalova, M. A., Chmielewski, M., Cicero, D. C., Conway, C., De Clercq, B., De Fruyt, F., Docherty, A. R., Eaton, N. R., Edens, J. F., Forbes, M. K., … Zimmermann, J. (2018). The time has come for dimensional personality disorder diagnosis. Personality and mental health, 12(1), 82–86. https://doi.org/10.1002/pmh.1408 usually involves:
- A physical examination of the patient
- Interviews with the patients and their families
- Psychological assessments
- Differential diagnosis of PD
If it is seen that the concerned patient is suffering from a personality disorder, he/she is advised medication and/or therapy. An early and timely diagnosis20 Widiger T. A. (2003). Personality disorder diagnosis. World psychiatry : official journal of the World Psychiatric Association (WPA), 2(3), 131–135. of a personality disorder means a better treatment outcome.
A psychologist or psychiatrist makes a differential diagnosis to separate out PD symptoms from similar symptoms associated with other psychiatric disorders like depression, psychosis, schizophrenia, etc. This is done through several personality disorder tests, such as:
- Standardized Assessment of Personality (SAP) 21 Walters, P., Moran, P., Choudhury, P., Lee, T., & Mann, A. (2004). Screening for personality disorder: a comparison of personality disorder assessment by patient and informants. International journal of methods in psychiatric research, 13(1), 34–39. https://doi.org/10.1002/mpr.162
- Structured Clinical Interview for DSM‐IV Personality Disorders (SCID‐II) 22 Farmer, R. F., & Chapman, A. L. (2002). Evaluation of DSM-IV personality disorder criteria as assessed by the structured clinical interview for DSM-IV personality disorders. Comprehensive psychiatry, 43(4), 285–300. https://doi.org/10.1053/comp.2002.33494
- Computerized Adaptive Test of Personality Disorder (CAT-PD) 23 Simms, L. J., Goldberg, L. R., Roberts, J. E., Watson, D., Welte, J., & Rotterman, J. H. (2011). Computerized adaptive assessment of personality disorder: introducing the CAT-PD project. Journal of personality assessment, 93(4), 380–389. https://doi.org/10.1080/00223891.2011.577475
- Minnesota Multiphasic Personality Inventory (MMPI) 24 Floyd AE, Gupta V. Minnesota Multiphasic Personality Inventory. [Updated 2022 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557525/ , etc.
Treatment For Personality Disorders
Personality disorders are complex and sometimes life-long psychiatric disorders. But these can be effectively managed by a combination of therapies, medications, and healthy self-help strategies.
Social support, as well as community awareness and aid, can go a long way for people recovering from crippling personality disorders. However, in severe cases, treatment for personality disorders involves hospitalization.
1. Therapy
Therapy for personality disorders addresses behavioral and conduct disorders 25 Bateman, A. W., Gunderson, J., & Mulder, R. (2015). Treatment of personality disorder. Lancet (London, England), 385(9969), 735–743. https://doi.org/10.1016/S0140-6736(14)61394-5 , self-harm and suicidal tendencies, and emotional dysfunction. In fact, these are aimed to induce empathy, assertiveness, confidence, and healthy thought processes in people suffering from personality disorders. The common therapies used in treating PDs include:
I. Psychotherapy
Psychotherapy improves the underlying, abnormal, psychological, and biological mechanisms that lead to a disordered personality. It helps the patients reorganize their thought processes and correct their behavior 26 Gabbard G. O. (2000). Psychotherapy of personality disorders. The Journal of psychotherapy practice and research, 9(1), 1–6. . Popularly, cognitive behavioral therapy 27 Bateman, A. W., Gunderson, J., & Mulder, R. (2015). Treatment of personality disorder. Lancet (London, England), 385(9969), 735–743. https://doi.org/10.1016/S0140-6736(14)61394-5 (CBT) and dialectic behavioral therapy (DBT) are used to treat personality disorders.
II. Mentalization-based treatment (MBT)
Mentalization-based treatment 28 Bateman, A., & Fonagy, P. (2010). Mentalization based treatment for borderline personality disorder. World psychiatry : official journal of the World Psychiatric Association (WPA), 9(1), 11–15. https://doi.org/10.1002/j.2051-5545.2010.tb00255.x is used to correct the reduced capacities to mentalize or self-reflect in people with PDs. It helps address problems related to emotional regulation and impulsivity, especially in the context of interpersonal interactions.
III. Milieu therapy
Milieu therapy 29 Belsiyal Chellappan, X., Rentala, S., & Das, A. (2021). Effectiveness of therapeutic milieu intervention on inpatients with depressive disorder: A feasibility study from North India. Perspectives in psychiatric care, 57(4), 1604–1615. https://doi.org/10.1111/ppc.12725 aims to address issues related to maladjustment in people suffering from personality disorders. It helps to make substantial changes in a patient’s immediate life circumstances and environment, reduce conflict and boost life satisfaction, and improve his/her quality of life.
IV. Family therapy
Family therapy 30 Glick, I. D., Dulit, R. A., Wachter, E., & Clarkin, J. F. (1995). The family, family therapy, and borderline personality disorder. The Journal of psychotherapy practice and research, 4(3), 237–246. aims to reduce conflict and ill feelings between people suffering from PDs and their close ones, especially family and friends. It addresses the broken or unsuccessful interpersonal relationships that characterize PDs.
V. Group therapy
Group therapy 31 Nehls N. (1992). Group therapy for people with borderline personality disorder: interventions associated with positive outcomes. Issues in mental health nursing, 13(3), 255–269. https://doi.org/10.3109/01612849209078777 involves patients with PDs joining groups of people suffering from similar personality disorders and resolving their issues by mutual understanding and empathy. It is the cornerstone of community support when it comes to recovery from crippling personality disorders.
2. Medication
Currently, there are no prescribed medications specifically for personality disorders. A 2018 study 32 Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235 elaborates that the current pharmacological treatment for personality disorders assumes that psychotropic drugs can treat the personality disorder symptoms specifically caused by biochemical abnormalities.
But, because of the diversity of symptoms and causes, medical practitioners have increasingly relied on psychiatric polypharmacy to address the symptoms of personality disorders.
For instance, in order to eliminate specific symptoms of comorbid psychiatric disorders in personality disorders (say borderline personality disorder), a combination 33 Olabi, B., & Hall, J. (2010). Borderline personality disorder: current drug treatments and future prospects. Therapeutic advances in chronic disease, 1(2), 59–66. https://doi.org/10.1177/2040622310368455 of antidepressants, antipsychotics, or mood-stabilizing drugs is administered. As heavy use of medication comes with risks of side effects, it is widely recommended that such a pharmacological treatment approach should come with close and continuous clinical supervision of medical specialists.
Coping With Personality Disorders
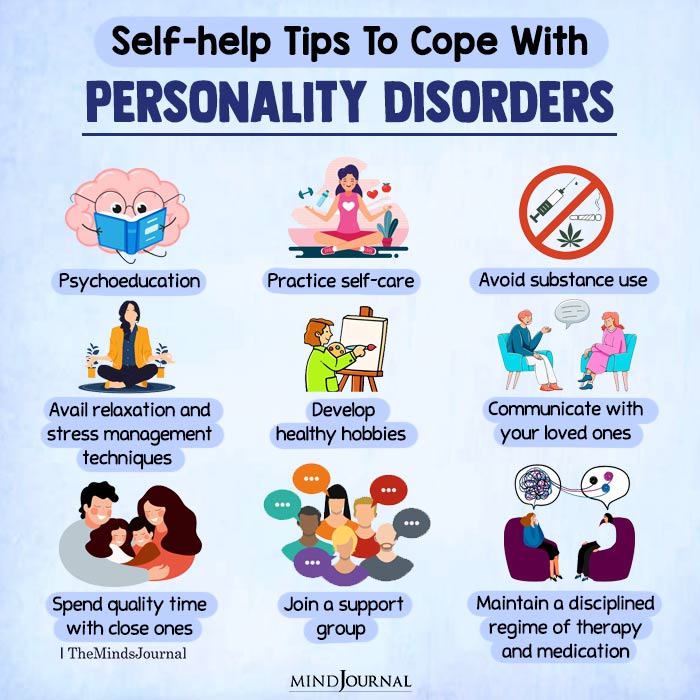
For people living with personality disorders, certain self-help strategies can help with day-to-day functioning. However, for severe personality disorders, it is always advisable to consult a psychologist or a psychiatrist as the symptoms may be unmanageable by the individual.
Consider the following self-strategies to cope with personality disorders:
- Educate yourself about personality disorders and how to address them
- Practice self-care by eating nutritious food, getting adequate sleep and exercise, etc.
- Avoid substance use (like alcohol, drugs, tobacco, etc.)
- Avail relaxation and stress management techniques like yoga, meditation, etc.
- Develop healthy hobbies that help you grow or practice gratitude (like journaling, gardening, hiking, etc.)
- Communicate with your loved ones and spend time with them
- Join a support group and develop a strong support system
- Maintain a disciplined regime of therapy and medication
- Identify your self-harm triggers and avail emergency mental health services, if needed
Takeaway
Personality disorders are perhaps some of the long-lasting, misunderstood, and crippling psychiatric disorders. If left untreated, these can go on to negatively impact a person’s quality of life, career, interpersonal relationships, and social functioning. However, they can be easily managed with therapy, medication, and self-help coping strategies, as well as by harboring faith and patience in the healing process.
Personality Disorders At A Glance
- Personality disorders (PDs) are manifestations of extreme personality traits that interfere with everyday life.
- Examples of personality disorders include antisocial PD, obsessive-compulsive disorder, borderline personality disorder, etc.
- PDs are of various types and can be divided into three clusters: A, B, and C.
- The causes of personality disorders are attributed to genetics and several psychosocial factors.
- If untreated, PDs can severely impair a person’s personal, professional, and social life.
- PDs can be effectively managed by a combination of therapies, medications, and healthy self-help strategies.
Frequently Asked Questions (FAQs)
1. Are personality disorders genetic?
Personality disorders are caused by a combination of genetic and environmental factors. Our genetics make us vulnerable to personality disorders, whereas environmental situations may trigger the actual development of the disorder.
2. What is the role of repressed childhood conflicts in personality disorders?
Most cases of personality disorders are attributed to childhood neglect and abuse and similar unresolved conflicts.
3. Can someone who has a personality disorder recognize it in others?
Personality disorders cause sufferers to have distorted perceptions of reality. They do not believe that anything is wrong with them. Therefore, the sufferers may not recognize their own troubling behavior and similar symptoms in others.
4. Do people with personality disorders fail to reveal their emotions?
People with personality disorders suffer from emotional dysfunction and they frequently struggle to identify emotions. This makes them unable to express emotions appropriately.
5. Are people living with personality disorders considered neurotypical?
Most people with mental disorders are not born with developmental disorders, and as such, they are considered neurotypical.
6. How does personality disorder relate to mental health?
Personality disorders are a category of mental disorders. They cause disturbances in a person’s mental health and wellbeing.
References:
- 1Newlin, E., & Weinstein, B. (2015). Personality disorders. Continuum (Minneapolis, Minn.), 21(3 Behavioral Neurology and Neuropsychiatry), 806–817. https://doi.org/10.1212/01.CON.0000466668.02477.0c
- 2Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235
- 3Fariba KA, Gupta V, Kass E. Personality Disorder. [Updated 2022 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556058/
- 4Sansone, R. A., & Sansone, L. A. (2011). Personality disorders: a nation-based perspective on prevalence. Innovations in clinical neuroscience, 8(4), 13–18.
- 5Tyrer, P., Mulder, R., Crawford, M., Newton-Howes, G., Simonsen, E., Ndetei, D., Koldobsky, N., Fossati, A., Mbatia, J., & Barrett, B. (2010). Personality disorder: a new global perspective. World psychiatry : official journal of the World Psychiatric Association (WPA), 9(1), 56–60. https://doi.org/10.1002/j.2051-5545.2010.tb00270.x
- 6Fariba KA, Gupta V, Kass E. Personality Disorder. [Updated 2022 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556058/
- 7Esterberg, M. L., Goulding, S. M., & Walker, E. F. (2010). Cluster A Personality Disorders: Schizotypal, Schizoid and Paranoid Personality Disorders in Childhood and Adolescence. Journal of psychopathology and behavioral assessment, 32(4), 515–528. https://doi.org/10.1007/s10862-010-9183-8
- 8Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235
- 9Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235
- 10Kacel, E. L., Ennis, N., & Pereira, D. B. (2017). Narcissistic Personality Disorder in Clinical Health Psychology Practice: Case Studies of Comorbid Psychological Distress and Life-Limiting Illness. Behavioral medicine (Washington, D.C.), 43(3), 156–164. https://doi.org/10.1080/08964289.2017.1301875
- 11Ramsay, G., & Jolayemi, A. (2020). Personality Disorders Revisited: A Newly Proposed Mental Illness. Cureus, 12(8), e9634. https://doi.org/10.7759/cureus.9634
- 12Sansone, R. A., & Sansone, L. A. (2011). Personality disorders: a nation-based perspective on prevalence. Innovations in clinical neuroscience, 8(4), 13–18.
- 13Nigg, J. T., & Goldsmith, H. H. (1994). Genetics of personality disorders: perspectives from personality and psychopathology research. Psychological bulletin, 115(3), 346–380. https://doi.org/10.1037/0033-2909.115.3.346
- 14Burns, S., Kappenberg, R., McKenna, A., & Wood, C. (1994). Brain injury: personality, psychopathology and neuropsychology. Brain injury, 8(5), 413–427. https://doi.org/10.3109/02699059409150993
- 15Widiger, T. A., Crego, C., Rojas, S. L., & Oltmanns, J. R. (2018). Basic personality model. Current opinion in psychology, 21, 18–22. https://doi.org/10.1016/j.copsyc.2017.09.007
- 16Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235
- 17Alarcón, R. D., & Foulks, E. F. (1995). Personality disorders and culture: contemporary clinical views (Part A). Cultural diversity and mental health, 1(1), 3–17.
- 18Candrian, M., Schwartz, F., Farabaugh, A., Perlis, R. H., Ehlert, U., & Fava, M. (2008). Personality disorders and perceived stress in major depressive disorder. Psychiatry research, 160(2), 184–191. https://doi.org/10.1016/j.psychres.2007.06.014
- 19Hopwood, C. J., Kotov, R., Krueger, R. F., Watson, D., Widiger, T. A., Althoff, R. R., Ansell, E. B., Bach, B., Michael Bagby, R., Blais, M. A., Bornovalova, M. A., Chmielewski, M., Cicero, D. C., Conway, C., De Clercq, B., De Fruyt, F., Docherty, A. R., Eaton, N. R., Edens, J. F., Forbes, M. K., … Zimmermann, J. (2018). The time has come for dimensional personality disorder diagnosis. Personality and mental health, 12(1), 82–86. https://doi.org/10.1002/pmh.1408
- 20Widiger T. A. (2003). Personality disorder diagnosis. World psychiatry : official journal of the World Psychiatric Association (WPA), 2(3), 131–135.
- 21Walters, P., Moran, P., Choudhury, P., Lee, T., & Mann, A. (2004). Screening for personality disorder: a comparison of personality disorder assessment by patient and informants. International journal of methods in psychiatric research, 13(1), 34–39. https://doi.org/10.1002/mpr.162
- 22Farmer, R. F., & Chapman, A. L. (2002). Evaluation of DSM-IV personality disorder criteria as assessed by the structured clinical interview for DSM-IV personality disorders. Comprehensive psychiatry, 43(4), 285–300. https://doi.org/10.1053/comp.2002.33494
- 23Simms, L. J., Goldberg, L. R., Roberts, J. E., Watson, D., Welte, J., & Rotterman, J. H. (2011). Computerized adaptive assessment of personality disorder: introducing the CAT-PD project. Journal of personality assessment, 93(4), 380–389. https://doi.org/10.1080/00223891.2011.577475
- 24Floyd AE, Gupta V. Minnesota Multiphasic Personality Inventory. [Updated 2022 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557525/
- 25Bateman, A. W., Gunderson, J., & Mulder, R. (2015). Treatment of personality disorder. Lancet (London, England), 385(9969), 735–743. https://doi.org/10.1016/S0140-6736(14)61394-5
- 26Gabbard G. O. (2000). Psychotherapy of personality disorders. The Journal of psychotherapy practice and research, 9(1), 1–6.
- 27Bateman, A. W., Gunderson, J., & Mulder, R. (2015). Treatment of personality disorder. Lancet (London, England), 385(9969), 735–743. https://doi.org/10.1016/S0140-6736(14)61394-5
- 28Bateman, A., & Fonagy, P. (2010). Mentalization based treatment for borderline personality disorder. World psychiatry : official journal of the World Psychiatric Association (WPA), 9(1), 11–15. https://doi.org/10.1002/j.2051-5545.2010.tb00255.x
- 29Belsiyal Chellappan, X., Rentala, S., & Das, A. (2021). Effectiveness of therapeutic milieu intervention on inpatients with depressive disorder: A feasibility study from North India. Perspectives in psychiatric care, 57(4), 1604–1615. https://doi.org/10.1111/ppc.12725
- 30Glick, I. D., Dulit, R. A., Wachter, E., & Clarkin, J. F. (1995). The family, family therapy, and borderline personality disorder. The Journal of psychotherapy practice and research, 4(3), 237–246.
- 31Nehls N. (1992). Group therapy for people with borderline personality disorder: interventions associated with positive outcomes. Issues in mental health nursing, 13(3), 255–269. https://doi.org/10.3109/01612849209078777
- 32Ekselius L. (2018). Personality disorder: a disease in disguise. Upsala journal of medical sciences, 123(4), 194–204. https://doi.org/10.1080/03009734.2018.1526235
- 33Olabi, B., & Hall, J. (2010). Borderline personality disorder: current drug treatments and future prospects. Therapeutic advances in chronic disease, 1(2), 59–66. https://doi.org/10.1177/2040622310368455